Intramural fibroids develop within the muscular wall of the uterus and are benign. They very rarely turn cancerous. According to Johns Hopkins Medicine, fibroids are quite common, affecting between 20-70 per cent of women during their reproductive years. The good news is that they’re almost always harmless, with an estimated more than 99% of cases being benign. Although women between 30 and 40 are most commonly affected, intramural fibroids can be seen even at an earlier age.. Often, they are found during pelvic exams.
This blog aims to give you insights into what exactly intramural fibroids are, along with their cause, symptoms and treatment options available today.
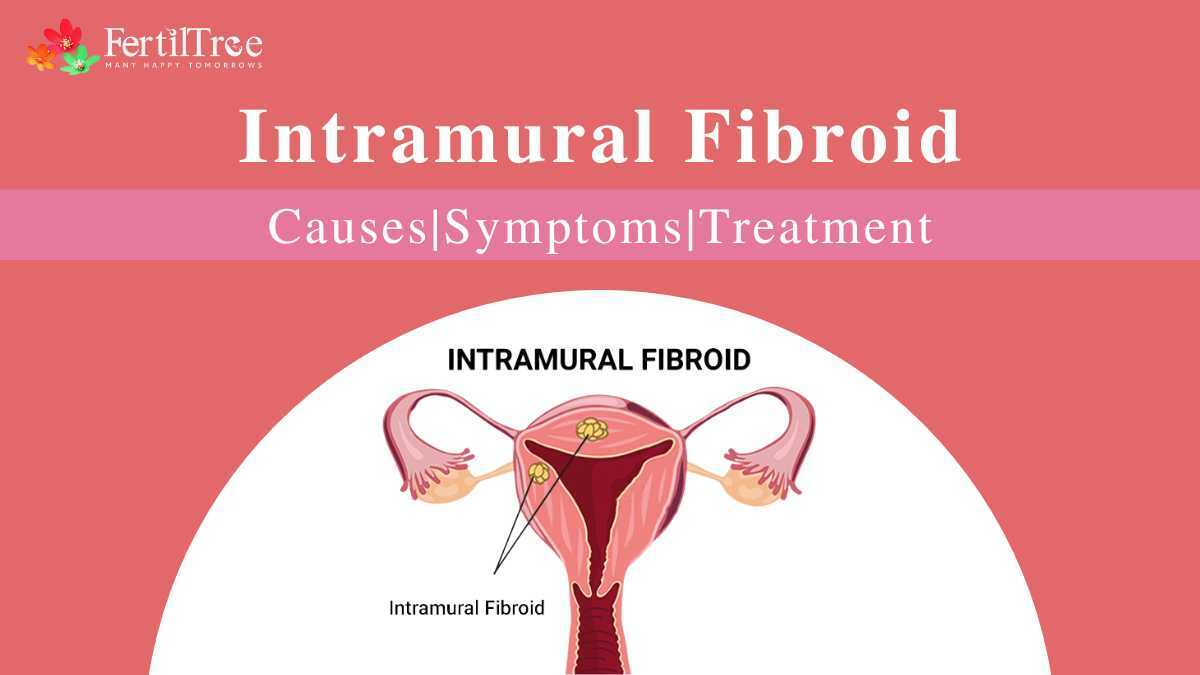
What Are Intramural Fibroids?
Intramural fibroids are frequently seen in the female reproductive system. These benign growths, composed of smooth muscle cells, develop within the muscular wall of a woman’s uterus. . They can vary in size and number, and while their presence might be concerning, it’s important to note they are non-cancerous.
Also Read: What is a Bulky Uterus?
Types Of Intramural Fibroids
While all intramural fibroids reside within the muscular wall of the uterus, their specific location can influence their impact and treatment approach. Below, you will find the 3 main intramural fibroid types:
| Type | Definition |
| Anterior Intramural Fibroids | These fibroids grow on the front wall of the uterus, facing the abdomen. |
| Posterior Intramural Fibroids | Located on the back wall of the uterus, these fibroids face the rectum. |
| Fundal Intramural Fibroids | They are found in the upper portion of the uterus, near the fundus. |
The location of a fibroid can determine the symptoms you experience. For instance, a large fibroid at the bottom of the uterus (fundal or posterior) might affect vaginal childbirth.
Also Read: Adenomyosis vs Uterine Fibroids: What’s the Difference?
Causes Of Intramural Fibroids
The exact cause of intramural fibroids remains elusive, but researchers have identified several contributing factors:
Genetic Factors:
Fibroids might have a family connection. Studies suggest that having a mother or sister with fibroids increases a woman’s risk.
Hormonal Influences:
Estrogen and progesterone also play a role in fibroid growth. Hormonal imbalances can trigger the development of intramural fibroids.
Environmental and Lifestyle Factors:
Consuming a diet high in red meat while steering clear of fruits and vegetables, along with obesity and physical inactivity, might contribute to fibroid development. More research is needed to confirm the exact link, but maintaining a healthy lifestyle is always beneficial.
Reproductive Factors:
Childbearing history seems to influence fibroid development. Women who haven’t given birth or had their first child later in life may be at a higher risk.

Symptoms Of Intramural Fibroids
While 80% of women might develop fibroids over the course of their reproductive span , the good news is that only a portion of these women will experience symptoms that require treatment. This means many women with fibroids live comfortably even without knowing they have them. However, if you do have fibroids or suspect that you do, it’s important to be aware of the potential symptoms. Following are some common signs lookout for:
- Heavy or Irregular Periods: This is a common sign, with periods becoming heavier or lasting longer than usual.
- Feeling Full or Bloated: A persistent feeling of fullness or bloating in the lower abdomen can be caused by larger fibroids.
- Frequent Urination: If a fibroid presses on your bladder, you might experience the urge to urinate more often, even if you haven’t consumed much fluid.
- Painful Intercourse: Depending on the location and size of the fibroid, sexual activity might become uncomfortable.
- Lower Back Pain: Any discomfort in the lower back can sometimes be a symptom of fibroids.
- Constipation: In some cases, fibroids can put pressure on the bowels, leading to constipation.
- Vaginal Discharge: Persistent vaginal discharge can be a symptom, though it’s important to note this could also be caused by other conditions.
- Swollen Belly: Large fibroids can sometimes cause the abdomen to appear swollen or distended.
Note: Remember, the above-mentioned symptoms can also be caused by other conditions. If you experience any of these concerns, consult your doctor for a proper diagnosis, and he will provide you with the right treatment plan accordingly.
When To Seek Medical Attention
While fibroids are typically benign, there are situations where consulting a doctor is crucial. If you experience any of the symptoms mentioned below, schedule an appointment with your doctor. They can provide a proper diagnosis, discuss your individual situation, and recommend the best course of action for you.
Impact On Reproductive Health
- Heavy Or Disruptive Periods: Excessive bleeding, periods lasting longer than usual, or severe anemia linked to heavy bleeding are all reasons to see a doctor.
- Pelvic Pain And Discomfort: Persistent pain or pressure in the lower abdomen or pelvic area warrants a doctor’s visit.
Pregnancy Concerns
- Struggles With Conception: If you’re facing challenges getting pregnant, fibroids could be a contributing factor. Consulting a doctor can help explore this possibility.
- Multiple Miscarriages: A history of miscarriages might be linked to fibroids. Discussing this with your doctor can be beneficial.
Postmenopausal Women
- Fibroid Diagnosis After Menopause: While fibroids usually shrink after menopause, a new diagnosis during this time necessitates a doctor’s visit to rule out any cancerous changes.
Diagnosis Of Intramural Fibroids
Early detection is imperative in order to manage fibroids effectively. Here’s a breakdown of the diagnostic tools doctors use to identify fibroids and differentiate them from other conditions:
1. Imaging Techniques:
- Ultrasound: This one is a non-invasive procedure that uses sound waves to bring images of the internal organs. There are two approaches commonly used:
- Transabdominal Ultrasound: A technician moves a probe over your abdomen to capture images of the uterus.
- Transvaginal Ultrasound: A slender probe is inserted into the vagina for a closer look at the uterus and surrounding structures.
- A 3D ultrasound image gives more information regarding the size, site and the nature of the fibroids.
- MRI Scan: This advanced imaging technique uses strong magnetic fields plus radio waves to generate detailed pictures of your pelvic region. An MRI scan can precisely determine the size, location, and number of fibroids.
2. Other Diagnostic Tests:
Hysteroscopy: During the hysteroscopy procedure, a thin, flexible instrument called a hysteroscope, which has a camera, is put in through the vagina and cervix into the uterus. This allows the doctor to see the inside of the uterine cavity and identify any abnormalities, such as fibroids. Sometimes, the doctor might take a tissue sample (biopsy) for further analysis during the hysteroscopy.
- Laparoscopy: In some cases, a laparoscopy might be recommended. This minimally invasive surgery includes making a small incision in the abdomen and then inserting a laparoscope (a thin, lighted tube) to examine the outside of the uterus and surrounding organs. Similar to a hysteroscopy, a biopsy might be performed during a laparoscopy if necessary.
Treatment Options For Intramural Fibroids
The course of treatment for intramural fibroids depends on various factors, like the size, the number, as well as the location of the fibroids, and the severity of your symptoms. Here’s an overview of the potential treatments:
- Medications
Medications are often the first line of treatment for managing intramural fibroids, especially when symptoms are mild. Here are some commonly used medications:
- GnRH Agonists: These drugs help shrink fibroids by reducing the body’s estrogen and progesterone production. They are typically used short-term and can cause menopause-like symptoms like hot flashes, sweating, and vaginal dryness. These are often administered before surgery to reduce fibroid size and ease the procedure.
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs): Medications like ibuprofen can alleviate pain associated with fibroids, but they do not reduce bleeding or shrink fibroids.
- Hormonal Birth Control: Oral contraceptives, intrauterine devices (IUDs) like Mirena, or progesterone injections such as Depo-Provera can help in regulating menstrual cycles and also reduce menstrual bleeding and pain without causing fibroid growth.
- Iron Supplements
For individuals experiencing heavy bleeding due to fibroids, iron supplements might be necessary to prevent or treat anemia. Heavy menstrual bleeding can, more often than not, lead to significant iron loss, resulting in fatigue and other anemia-related symptoms.
- Gonadotropin-Releasing Hormone (GnRH) Agonists
GnRH agonists are a more specific type of medication used to shrink fibroids temporarily. These medications induce a state similar to menopause, reducing estrogen levels, which in turn causes fibroids to shrink. They are usually prescribed before surgical procedures to make fibroid removal easier and less invasive.
- Surgery for Fibroids
When medications are not effective or suitable, surgical options may be considered. Surgery can be more definitive in addressing fibroids and providing symptom relief. Here are some surgical treatments for intramural fibroids:
Myomectomy
Myomectomy is a type of surgical procedure that removes fibroids while still preserving the uterus. It is ideal for individuals who wish to maintain fertility. There are different approaches to myomectomy.
- Hysteroscopy: This involves inserting a thin, flexible surgical tool through the vagina and cervix to remove fibroids.
- Laparoscopy: A minimally invasive procedure where fibroids are removed using small incisions in the abdomen.
- Laparotomy: A more invasive approach involving a larger abdominal incision to remove fibroids.
Hysterectomy
During a hysterectomy, the uterus is removed. It is considered in older women, when fibroids are large, causing severe symptoms, or if future pregnancy is not a consideration. This procedure is the only definitive cure for fibroids, as it completely eliminates the possibility of recurrence.
Uterine Fibroid Embolization (UFE)
UFE is a minimally invasive procedure where an interventional radiologist injects small particles into the uterine arteries to stop or block blood flow to the fibroids, which cause them to shrink. This procedure is not suitable for those who wish to maintain fertility but is effective in reducing or eliminating fibroid symptoms in many cases.
Radiofrequency Ablation (RFA)
RFA is a less invasive approach that uses microwave energy to heat and destroy fibroid tissue. It is effective for smaller fibroids and can be performed on an outpatient basis.
Lifestyle and Home Remedies
While medical intervention plays a role in managing fibroids, adopting a healthy lifestyle can significantly improve your overall well-being and potentially alleviate symptoms. Here are some key things you can proactively do by yourself:
Diet And Nutrition: Maintaining a healthy weight can be beneficial, as excess estrogen in fatty tissues might contribute to fibroid growth. Focus on a well-balanced diet that is preferably rich in fruits, vegetables, and whole grains. These foods provide essential nutrients and fibre, which can help regulate hormones and improve your health altogether. Also, consider reducing red meat intake and opt for leaner protein sources like fish, poultry, or legumes. Processed foods often have high levels of unhealthy fats, sodium, and preservatives, so it’s best to limit them as well.
Exercise And Physical Activity: Aim for 30 minutes of moderate-intensity exercise at the very least most days of the week. Walking, swimming, biking, and yoga are all excellent options. Try out strength training exercises in your routine daily can help build muscle mass, which can further aid in weight management and overall hormone regulation. Try and start with lighter weights and then you can gradually increase intensity as you get stronger.
Stress Management Techniques: While the exact link isn’t fully understood, stress can worsen fibroid symptoms. Explore relaxation techniques like yoga, meditation, deep breathing exercises, or spending time in nature.
Read more: Foods To Increase Sperm Count and Motility
Complications Of Untreated Intramural Fibroids
While many women with intramural fibroids experience no symptoms or minimal discomfort, leaving them untreated can sometimes lead to complications.
- Heavy or Prolonged Menstrual Bleeding: This one is a common consequence, leading to fatigue and anemia due to iron deficiency.
- Pelvic Pain and Pressure: Large fibroids can press on surrounding organs, causing persistent pain or a feeling of fullness in the lower abdomen.
- Urinary Issues: Fibroids pressing on the bladder might lead to frequent urination or difficulty in emptying the bladder completely.
- Painful Intercourse: Depending on the location and size of the fibroids, sexual activity might become uncomfortable.
- Infertility: In some cases, fibroids can obstruct the fallopian tubes or create an unfavourable environment for implantation, hindering pregnancy. However, this doesn’t apply to all women with fibroids.
- Fast-Growing or Large Fibroids: Untreated, fibroids might grow larger, potentially causing more severe symptoms and requiring more complex treatment options in the future.
Read more: Steps to Getting Pregnant With Blocked Fallopian Tubes
Prognosis And Long-term Outlook
Thankfully, having intramural fibroids doesn’t have to hold you back. Here’s an optimistic outlook:
- Positive Prognosis: With proper management, the outlook for women with fibroids is generally good. Most fibroids are benign and pose no serious health threat.
- Symptom Management: While fibroids can cause unpleasant symptoms, there is a plethora of treatment options available to address them effectively. Talking to your doctor can help you find the best approach to managing your specific situation.
- Treatment Tailored to You: From medications and minimally invasive procedures to even surgery, various options can be explored to find the most suitable solution for your individual needs and future plans.
Success Rate Of Treating Intramural Fibroids
Success rate depends on many factors. The age of the woman, the size, shape, position, vascularity and position of the fibroids and other associated conditions like presence of endometriosis and adenomyosis.
Conclusion
While the exact causes of intramural fibroids remain unclear, Genetic, hormonal, environmental, and lifestyle factors contribute to their development. They can cause different kinds of symptoms, including heavy periods, pelvic pain, and fertility issues, though many women may remain asymptomatic. Early detection and timely treatment of intramural fibroids are of absolute importance to prevent complications and improve your quality of life. Regular pelvic exams and awareness of symptoms can lead to prompt medical intervention and can even reduce the risk of severe anemia, chronic pain, and reproductive issues.
Found this post informative? Read more insightful Blogs at FertilTree. For expert guidance on fertility treatments, visit Dr. Firuza Parikh’s profile and explore the wealth of resources available on FertilTree.
For further inquiries, you can reach out to us at [email protected] or call us at +91-22-66573175.
Read More:
FAQs on Intramural Fibroid
Why do intramural fibroids occur?
What are the main causes of fibroids?
What is the best treatment for intramural fibroids?
Can intramural fibroids go away on their own?
Is it necessary to remove intramural fibroids?
Can a woman live with fibroids?
How do you treat fibroids without surgery?
Medications: Medications like GnRH agonists and antagonists can shrink fibroids or regulate bleeding.
Uterine Fibroid Embolization (UFE): This minimally invasive procedure cuts blood flow to the fibroids, causing them to shrink.
Radiofrequency Ablation (RFA): This procedure uses heat to destroy fibroid tissue.
Is intramural fibroid harmful?
What size intramural fibroid needs surgery?
What are the signs of fibroid shrinking?
Is it okay to live with fibroids?
Sources:
Eltoukhi, Heba M., et al. “The Health Disparities of Uterine Fibroid Tumors for African American Women: A Public Health Issue.” American Journal of Obstetrics and Gynecology, vol. 210, no. 3, Mar. 2014, pp. 194–199, www.ncbi.nlm.nih.gov/pmc/articles/PMC3874080/, https://doi.org/10.1016/j.ajog.2013.08.008.
Pandey, Dr Mayuri. “Intramural Fibroid: Symptoms, Diagnosis, and Treatment.” PharmEasy Blog, 24 May 2023, pharmeasy.in/blog/diagnostics-intramural-fibroid-symptoms-diagnosis-treatment/. Accessed 17 June 2024.
“Https://Www.narayanahealth.org/Blog/Intramural-Fibroid-Causes-Symptoms-And-Treatment-Options.” Narayana Health, www.narayanahealth.org/blog/intramural-fibroid-causes-symptoms-and-treatment-options. Accessed 17 June 2024.
“Uterine Fibroids: Q&a with an Expert.” Www.hopkinsmedicine.org, www.hopkinsmedicine.org/health/conditions-and-diseases/uterine-fibroids-qa-with-an-expert#:~:text=Fibroids%20are%20pretty%20common%20%E2%80%94%20between.
Book A Consultation