Did you know that younger women have a higher chance of having healthy eggs? Studies show that women in their early 20s have a very good chance, around 80%, of having eggs that can develop into healthy embryos. This change decreases with age, but there are still options for those looking to conceive later in life.
The quality of a woman’s eggs plays quite a pivotal role in fertility. What many people don’t know is that high-quality eggs are essential for successful fertilization, implantation, and the development of a healthy pregnancy. Unfortunately, not all eggs possess the same potential and poor egg quality can pose significant challenges for those trying to get pregnant. This blog aims to provide you with all the necessary information about poor egg quality, including its symptoms, causes, and available treatment options.
Table of Contents – Signs of Poor Egg Quality
Understanding Egg Quality
When we say egg quality, it refers to the egg’s ability to be fertilized and develop into a healthy embryo. Eggs that are of high quality have the correct chromosome number, and effectively result in a healthy embryo and pregancy.It’s important to remember that as women age, egg quality declines, further impacting fertility. However, other factors besides age can also affect egg quality, and we will take a closer look at those in this blog.
What Does Poor Egg Quality Mean?
Poor egg quality means that the eggs have a compromised ability to be fertilized and develop into healthy embryos. This is a significant factor in female infertility and is often linked to age, genetics, hormone imbalances, and environmental factors. Symptoms of poor egg quality can include infertility issues, frequent miscarriages, and irregular menstrual periods. Addressing poor egg quality involves lifestyle changes, dietary adjustments, advanced reproductive technologies like IVF, and sometimes egg donation.
Read more: How To Improve Egg Quality After 40
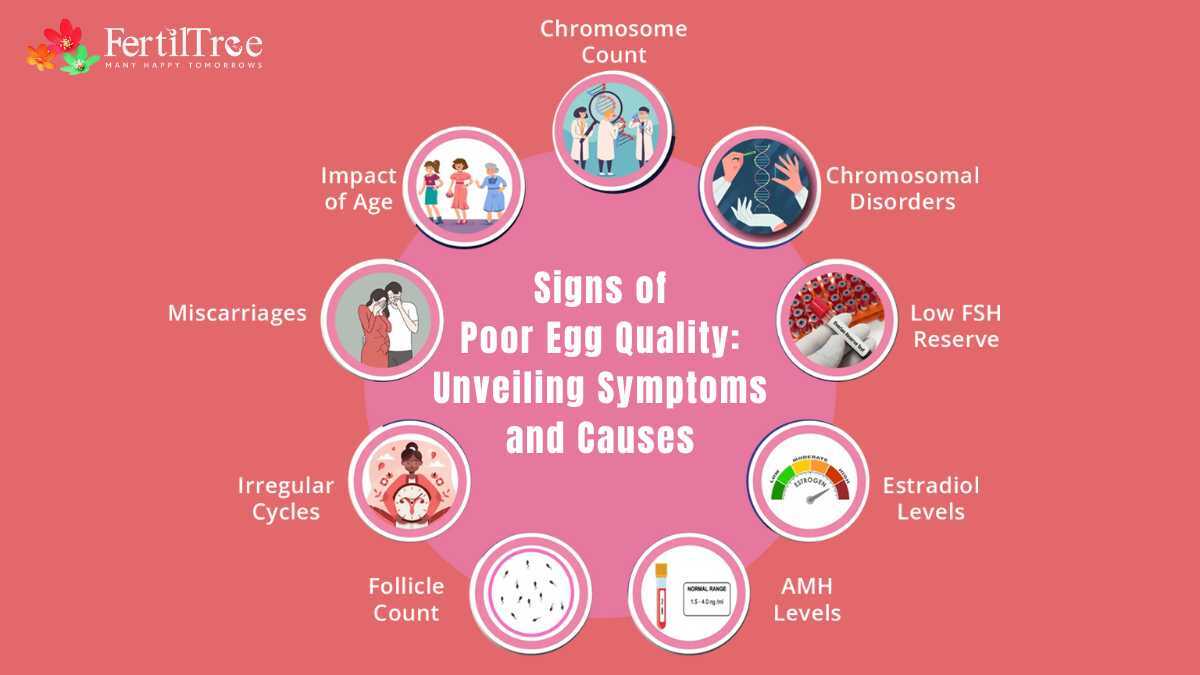
Signs of Bad Egg Quality in Fertility
Signs to lookout for include:
- Irregular Periods: Inconsistent menstrual cycles can indicate hormonal imbalances that affect egg quality.
- Repeated Miscarriages: Frequent pregnancy losses may be due to chromosomal abnormalities in the eggs.
- Age: Women over 36 are more likely to experience a decline in egg quality.
- Low FSH Reserves: Low levels of follicle-stimulating hormone can suggest poor ovarian function.
- Low Estradiol Levels: Insufficient estradiol can impair the preparation of the uterine lining for implantation.
- Low AMH Levels: Low anti-Müllerian hormone levels indicate a reduced ovarian reserve.
- Low Follicular Count in Sonography: Fewer follicles seen on an ultrasound scan may suggest diminished egg quantity and quality.
- Chromosomal Disorders: Eggs with chromosomal abnormalities are less likely to result in successful healthy pregnancies.
Read more: Can You Lower My FSH Level?
What Are Some Causes of Poor Egg Quality?
A number of factors play a role in egg quality becoming poor, and here are some of the known and common ones:
1. Age: The primary factor, with fertility declining sharply after age 35 due to increased incidence of abnormal eggs.
2. Genetic Factors: Inherited conditions or genetic mutations can affect ovarian function and egg development.
3. Environmental Stressors: Exposure to pollutants, toxins, or radiation can induce oxidative stress and damage eggs.
4. Lifestyle Choices: Poor diet, smoking, excessive alcohol consumption, and lack of sleep can negatively impact egg quality.
5. Hormonal Imbalances: Hormonal irregularities in FSH/LH TSH Prolactin and AMH, can disrupt egg development.
6. Medical Conditions: Medical conditions, including polycystic ovary syndrome (PCOS) and endometriosis, elevated cholesterol and high blood sugar can impair egg quality.
Read more: Empty Follicle Syndrome
The Impact of Bad Egg Quality on Fertility
Women’s ovaries are programmed to release one egg per menstrual cycle. If the released egg is of poor quality, it may not fertilize or implant properly, leading to infertility or miscarriage. Poor egg quality can also result in embryos with chromosomal abnormalities, increasing the risk of conditions like Down syndrome. This is why fertility naturally declines with age, and issues like miscarriage and genetic disorders become more common in women over 35.
How To Improve Women’s Egg Quality?
There are a few things that you can do to improve the quality of your eggs, and they include:
- Prioritize Nutrient-Rich Foods: A diet rich in antioxidants, vitamins, and minerals can protect eggs from oxidative damage. Incorporate leafy greens, berries, nuts, seeds, oily fish, and whole grains into your meals.
- Maintain a Healthy Weight: Both underweight and overweight women may experience disruptions in their menstrual cycles and hormone levels, affecting egg quality. You must aim for a healthy body mass index (BMI) by embracing a balanced diet and regular exercise.
- Manage Stress Levels: Chronic stress can disrupt hormone balance and affect egg quality. Practice stress-reducing activities like yoga, meditation, deep breathing exercises, or spending time in nature.
- Avoid Harmful Substances: Minimize exposure to tobacco, alcohol, and recreational drugs. Smoking decreases ovarian reserve, while excessive alcohol consumption can impair reproductive function.
- Consider Supplements and Herbs: Supplements like CoQ10 and myoinositol may help improve egg quality and ovarian function. Berries and Maca root have been used to support reproductive health. Talk to your doctor first before starting any new supplements.
What Are Some Treatment Options for Poor Egg Quality?
If you’re facing challenges due to poor egg quality, there’s hope. Here are some treatment options:
- Advanced Reproductive Technologies (ART): Techniques like IVF and ICSI and Preimplantation Genetic Testing can help by selecting the healthiest embryos for implantation.
- Ovarian Reserve Assessment and Management: Early detection and management of diminished ovarian reserve can optimize ovarian function and improve egg quality.
- Holistic Approach: Fertility specialists may recommend a holistic approach that addresses lifestyle factors impacting egg quality.
- Donor Egg Programs: For severe egg quality issues, donor egg programs offer an alternative path to parenthood. FertilTree has an ongoing Oocyte Donation Program, wherein donors undergo thorough physical, medical, and genetic screening to ensure the highest standards.
- Tailored Treatment Plans: Experienced fertility specialists will personalize treatment plans as per your unique needs as well as your situation.
Read more: Top Foods to Improve Female Egg Quality
Diagnostic Tests for Egg Quality
There are several tests that can provide insights into egg quality and ovarian reserve:
- AMH Testing: The AMH test estimates the number of eggs remaining in the ovaries.
- FSH Testing: This blood test measures follicle-stimulating hormone, which can indicate ovarian function.
- Estradiol Testing: This blood test measures estradiol, a hormone produced by egg follicles.
- Antral Follicle Count: This ultrasound scan counts the follicles in the ovaries, which can be an indicator of egg reserve.
Read More: Egg Freezing Process in India
Found this post informative? Read more insightful Blogs at FertilTree. For expert guidance on fertility treatments, visit Dr. Firuza Parikh’s profile and explore the wealth of resources available on FertilTree.
For further inquiries, you can reach out to us at [email protected] or call us at +91-22-66573175.
FAQs on Signs of Poor Egg Quality
Is irregular menstruation always a sign of bad egg quality?
How often should I get tested for egg quality?
Can poor egg quality be improved?
Is age the primary factor affecting egg quality?
How does stress affect egg quality?
What is the success rate of IVF for those with poor egg quality?
Are there any natural ways to improve egg quality?
Is bad egg quality the sole reason for repeated miscarriages?
How does low AMH affect fertility?
Can environmental toxins affect egg quality?
Can you conceive with poor egg quality?
Does poor egg quality mean birth defects?
Sources:
admin. “Poor Egg Quality : Symptoms, Causes, and Treatment.” ART Fertility Clinic, 25 Nov. 2023, www.artfertilityclinics.com/in/en/art-blog/poor-egg-quality-symptoms-causes-treatment. Accessed 10 June 2024.
Chang, Yajie, et al. “Egg Quality and Pregnancy Outcome in Young Infertile Women with Diminished Ovarian Reserve.” Medical Science Monitor, vol. 24, 12 Oct. 2018, pp. 7279–7284, https://doi.org/10.12659/msm.910410.
Book A Consultation