Preimplantation Genetic Testing In Mumbai, India
Preimplantation Genetic Testing (PGT) helps you screen for genetic disorders
There are many benefits to using FertilTree's PGT services, mainly to identify embryos that are at risk for developing chromosomal abnormalities. This information is precious for couples who are considering fertility treatment, as it can help them make informed decisions about which embryos to implant.
Utility of PGT:
Improves pregnancy rates and decreases spontaneous miscarriages in:
- Older age women
- Previous unsuccessful IUI/IVF attempts
- History of recurrent spontaneous miscarriages
- Male factor infertility
- History of repeated terminations because of an abnormality in the fetus.
- Known carriers of a genetic defect (e.g. Beta-Thalassemia, Sickle cell anemia, Cystic
Fibrosis, Spinal Muscular Atrophy, Duchenne Muscular Dystrophy, Fragile X Syndrome,
Huntington Chorea or chromosomal translocation.
Benefits of PGT:
- It prevents chromosomally or genetically abnormal births in couples with a failed fertilisation history after IVF-ICSI, missed abortions or carriers of balanced translocations.
- Increases the chances of implantation
- Decreases the time of pregnancy (TTP).
- Reduces the incidence of spontaneous miscarriages.
- Reduces the incidence of multiple offspring.
- Eliminates the risk of a child being affected with a familial gene disorder.
- A previously affected child can be cured by a Saviour Sibling (HLA matched sibling)
who can donate the stem cells to the affected child. E.g. Thalassemia major.
What is Preimplantation Genetic Testing

Preimplantation Genetic Diagnosis (PGD) now termed Preimplantation Genetic
Testing (PGT) is the earliest form of prenatal diagnosis. A single cell or a few cells are removed (biopsied) from the embryo obtained using IVF technology and checked for specific genetic abnormalities. The embryos that are reported normal are transferred into the mother’s uterus. PGT offers a new alternative to chorionic villus sampling or amniocentesis. PGT testing requires multiple embryos developed by ICSI.
(A) PGT FOR ALL 24 CHROMOSOME ANEUPLOIDIES (PGS OR PGT-A) Preimplantation Genetic Screening (PGS), also called Preimplantation Genetic Testing for Aneuploidy (PGT-A), checks for the number of chromosomes and any major gain or loss of genetic material in the chromosomes.
What are chromosomes?

Chromosomes which are present in the nucleus of the cell, contain the genetic material of the cell. Chromosomes contain DNA. Our DNA is organized into small structures called genes. These influence our growth and development. Genes are transmitted from parent to offspring and are considered to be the basic units of inheritance.
Forty-six chromosomes are present in all human cells except the gonadal cells (eggs and sperm). The egg and the sperm each have 23 chromosomes, of which 22 are autosomes, and 1 is the sex chromosome. In the egg, the sex chromosome is always X. In each sperm, the sex chromosome can be either X or Y. When the egg and sperm unite at fertilization, the number of chromosomes becomes 46. Depending on which sperm fertilises the egg, the embryo becomes male (XY) or female (XX).
In each embryo, chromosomes 1 to 22 are in 2 copies, where one comes from the sperm (biological father) and the egg (biological mother). Thus, an embryo with 46 chromosomes (22 pairs of autosomes and one pair of sex chromosomes) is considered a euploid (Normal) embryo.
When the number of chromosomes alters, the embryo is aneuploid (Abnormal). Monosomy occurs when there is a loss of 1 copy of the chromosome from the pair. When an extra copy is present, it is called trisomy of that particular chromosome. When the entire set of 23 chromosomes is extra, it is called triploidy. When both sets of 23 chromosomes are extra, it is called tetraploidy. If the copy number is more than 4, it is called polyploidy. If only 1 set of chromosomes (23) is present, it is called haploidy. If more than one cell line is current, one with 46 chromosomes and the other with more or less than 46, it is called
mosaicism. Mosaicism can occur during embryonic division.
Aneuploidies of embryos can result in spontaneous miscarriages, stillbirths, or developmental disorders in children. The most common aneuploidies are of chromosomes 13, 18, 21, X and Y, followed by aneuploidies of chromosomes 16 and 22.
(B) PGT FOR STRUCTURAL REARRANGEMENTS (PGS OR PGT-SR)
A chromosome translocation is a chromosome abnormality caused by the rearrangement of parts of 2 different chromosomes. Translocations can be balanced (an exchange of material with no extra or missing genetic information) or unbalanced (where during the exchange of chromosome material, there can be extra or missing genes, and normal functionality is affected). Couples with balanced translocations have a 25% chance of having a child with normal chromosomal make-up and a 25% chance of having a child with balanced translocation (fully functional). There is a 50% risk of having a child with unbalanced translocation, which may lead to miscarriage, Intrauterine growth restriction (IUGR), Intrauterine fetal death (IUFD) or
delayed developmental milestones.
(C) PGT FOR MONOGENIC DISORDERS (PGT-M):
Just like chromosomes come in pairs, most genes come in pairs, one from the egg and one from the sperm. When the function of a gene is altered by a change (called a mutation) in the specific sequence of the DNA, a genetic disease results; these mutations can be transmitted in families from generation to generation (inherited) or can be a new change in an individual (de novo). These mutations lead to either single gene or multiple gene disorders.
Genetic diseases can be inherited in different ways. A dominant genetic disease is caused by a mutation in one copy of a gene. The risk for a parent with the disease to pass on the condition to the child is 50%. e.g. Huntington’s Chorea.
A recessive genetic disease is caused by a mutation in both copies of a gene. A carrier has one normal copy of the gene and one copy with a mutation. Most of them are healthy since having one normal copy is enough to prevent the disease. Two carrier parents have a 25% risk to have a child with the genetic disease. e.g. Thalassemia, Cystic Fibrosis.
Sex-linked genetic diseases are caused by mutations on the X or Y chromosomes. Sex-linked diseases can be dominant or recessive and affect males and females differently. In some genetic diseases, the abnormality in the gene keeps increasing in the next generation and its expression is seen only when an affected child is born. e.g. Fragile X Syndrome. Hence, if there is any history of having an affected child, it is
advisable to undergo testing in the next pregnancy and also test other family members.
The creation of a “saviour sibling” involves the selection of an embryo (via HLA typing and PGT) that, when born, could provide umbilical cord stem cells or bone marrow stem cells to an older sibling suffering from a serious medical condition that is amenable to treatment by such a donation. PGT-M with HLA matching for this purpose is suitable because only a limited number of HLA-matched unaffected embryos are transferred back, so this serves as a saviour sibling for the affected child who needs a transplant later on.
Preimplantation Genetic Testing is carried out for couples who are at high risk for various genetic disorders, those with male factor infertility, advancing maternal age or repeated failed IVF and repeated miscarriages. PGT-M is also performed for genetic conditions such as Thalassemia, Sickle Cell Disease, Duchenne Muscular Dystrophy, Leigh Syndrome, Huntington’s Disease, Neurofibromatosis, Cystic Fibrosis and Hereditary Cancer Predisposition Syndromes. PGT-M is also helpful to get HLA- matched unaffected embryos to create a saviour sib to cure a previously affected child with haematological disorders.
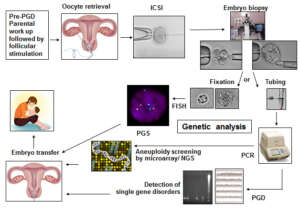
Steps involved in the PGT cycle:
For PGT testing, multiple embryos are developed by performing ICSI. The steps involved in PGT are:
- Pre-PGT work-up:
For the couple opting for PGT for single gene disorders (PGT-M), it is important to carry out Genetic testing for the disorder in both partners prior to PGT-M. This determines the mutation (alteration in genetic material) status of both partners. Based on the genetic report, the actual PGT protocol is developed. PGT for single gene disorders (PGD/PGT-M) is carried out only for the known disorder and mutation which is identified for the couple. Other unknown genetic abnormalities cannot be tested at this time.
Other important genetic tests for PGT/PGD/PGS:
- Karyotyping: Chromosomal analysis is carried out to check for aneuploidy, translocation or the presence of mosaicism.
- Sperm FISH to check for a percentage of aneuploid sperm. (i.e. sperm with an abnormal number of chromosomes)
- Sperm DNA Fragmentation Index to check for the percentage of sperm with DNA fragmentation.
Many routine blood parameters are also tested. Once these reports are ready, the ovarian stimulation cycle begins.
- Hormonal stimulation and oocyte retrieval: The female partner undergoes ovarian stimulation using hormones in order to obtain an adequate number of eggs. The eggs are collected under mild anesthesia.
- ICSI/ IMSI: ICSI (Intracytoplasmic sperm injection) is performed. A single sperm is injected into the
cytoplasm of the mature egg. After fertilization, the embryo is further incubated in culture up to Day 5/Day 6/Day 7.
- Embryo biopsy at the Blastocyst stage: For chromosomal aneuploidy screening (PGS / PGT-A) and for single-gene disorders (PGD / PGT-M), the embryo biopsy is done on Day 5 or Day 6 (Blastocyst Stage).
The Blastocyst is made up of a cluster of cells called the Inner Cell Mass (ICM): which forms the fetus and the trophectoderm cells (which form the placenta). By gentle micromanipulation about 5-8 trophectoderm cells are aspirated into a pipette, loaded into a tube and sent for genetic analysis.
All of the above steps are carried out in the Embryology Laboratory. The trophectoderm cells are then transported to the Genetics Lab for further testing. After the biopsy, the embryos are cryopreserved till the day of embryo transfer.
▪ Different techniques of genetic testing include Fluorescence in Situ Hybridization (FISH), Array Comparative Genomic Hybridization (aCGH) and Next Generation Sequencing (NGS).
▪ Embryo transfer of the genetically normal embryos is carried out in a frozen embryo transfer (FET) cycle and sometimes in the same cycle by doing a quick run analysis.
▪ A pregnancy test is performed 14 days later.
Techniques offered at our IVF Centre in Mumbai:
1. PGT for structural rearrangements (PGS or PGT-SR) by Fluorescence In Situ Hybridization (FISH) for telomeric/cryptic translocations and inversions
PGT by the FISH technique is now mainly carried out in cases where the husband or wife is a carrier of a balanced translocation or inversion. This is required to select embryos free of related unbalanced rearrangements. Pre-PGT work-up of the couple using specific probes for the rearrangements is necessary to check for an additional tiny or cryptic rearrangement which may not have been noticed earlier. The embryo biopsy is done on Day 5. About 4-8 trophectoderm cells are biopsied from each embryo and are fixed on slides and subjected to the FISH procedure using probes specific for each couple, as per the chromosomes involved. The fluorescent signals are observed using the fluorescent microscopy technique. A normal cell will show two signals of each colour for each chromosome. If there are 3 signals or 1 signal present, it indicates abnormal embryos which are not transferred to the mother.
Our team has 22 years of experience in such cases and has reported the first live births for Robertsonian /Reciprocal translocations and inversions in India.
2. PGT for all 24 chromosome aneuploidies (PGS or PGD-A) using the array Comparative Genomic Hybridization (aCGH) technique:
For 24 chromosome PGT, the biopsied cells are “tubed” and the DNA is amplified and tested for chromosomal aneuploidies using the microarray technique. Detection of all 24 chromosomes is possible on Day 5 of embryonic development. The results are available within 24 hours. The technique can also be used for the detection of unbalanced translocations except those involving the telomeres (tips) of the chromosomes.
3. PGT for all 24 chromosomal aneuploidies (PGS or PGT-A) using Next Generation Sequencing (NGS):
For PGT, the biopsied cells are “tubed”. The embryonic DNA is further subjected to a series of procedures and is finally sequenced using NGS technology to check for chromosomal aneuploidies. Detection of all 24 chromosomes is possible on Day 5 of embryonic development. The results are available within 24 hours.
4. PGT for single-gene disorders (PGT-M or PGD):
Whole-genome amplification is carried out to increase the quantity of DNA externally in a PCR machine. Then the amplified product is subjected to further testing for the single gene disorder. The parental genetic markers are matched with the embryonic markers in order to make a diagnosis.
Please note that our centre does not perform any form of sex determination by PGT in any form.
Our achievements after Preimplantation Genetic Diagnosis (PGS/PGD):
- A female baby was born by PGD using the FISH technique for Robertsonian translocation t(13;14). This is the first report from India.
- The live birth of a female child born after IVF followed by PGD using the FISH technique for Reciprocal translocation t(6;19). This is the first report from India. F. R. Parikh. (2012). Reproductive BioMedicine Online, 21:Suppl. 2, P15, S51.)
- Twin pregnancy and delivery after IVF followed by PGT for inversion 12 with t(9;12)
- First successful twin delivery in India after Preimplantation Genetic Diagnosis for the BRCA1 mutation. as on? additional Cryptic abnormality.
- First successful twin delivery in India after Preimplantation Genetic Diagnosis for the BRCA1 mutation.
- We offer PGT for different single-gene disorders such as beta-thalassemia, sickle cell anaemia, Huntington chorea, Duchenne muscular dystrophy, Norries disease, Leigh Syndrome, Retinoblastoma, etc. We also offer PGT to select HLA-matched unaffected embryos in blood disorders such as beta-thalassemia and Fanconi anaemia, to cure an affected sibling.
Risks and Limitations:
Even though the benefits of PGT-M/PGT-A are considerable, some risks and limitations have to be kept in mind. This procedure cannot guarantee a healthy pregnancy or eliminate the risk of miscarriage, stillbirth or the birth of a child with an abnormality.
- If less number of oocytes are retrieved, the ICSI cycle may have to be repeated.
- Occasionally there may be decreased fertilization, few healthy embryos or embryos that cleave slowly and do not reach the Blastocyst stage. Hence a biopsy may not be possible.
- If the quality of the embryo is poor, the genetic material present in the biopsied cells may be degraded causing breaks in the cellular DNA. Such DNA material may not give results. In such a case, a repeat trophectoderm biopsy may be needed.
- It is possible that all the embryos may show genetic abnormalities and hence embryo transfer may not be possible.
Why is IVF required for PGT even when the couple is fertile?
To test the embryonic cells using PGT before implantation for any genetic condition, the embryos should be available outside the body at a very early stage for testing before implantation. Also, more embryos need to be tested for any genetic disorder in order to get at least one unaffected embryo. This is possible using IVF as this allows the creation of multiple embryos.
Why should I choose FertilTree?
There are many reasons to choose FertilTree for Preimplantation Genetic Testing. First and foremost, our team has 22 years of experience with PGT and is fully qualified to provide this type of testing. We have a wealth of knowledge and experience in fertility treatment and protocols, and we’re passionate about helping our patients achieve their goals.
In addition, we offer a comprehensive range of services under one roof. This means that you can come to us for all your fertility needs, from initial consultation and testing through to treatment and post-treatment care. We’ll be with you every step of the way, ensuring that you receive the highest standard of care possible.
Cost of Preimplantation genetic testing (PGT) in India
The cost for preimplantation genetic testing (PGT) in India depends on the genetic abnormality to be tested. It can be only chromosomal aneuploidy or a single gene disorder or multiple gene disorders. It varies on a case-to-case basis depending on the medical condition and, suitability. It also includes an ICSI cycle and costs for the genetic disorder to be tested.