Genetic Disorders
Karyotyping from blood can be carried out for all age groups.
Indications for cytogenetic analysis:
Children with-
- Dysmorphic features
- Developmental delay
- Congenital anomalies
- Ambiguous genitalia
- Hypogonadism / undescended testes / hypospadias
- Delayed menarche and short stature
Sample: 2-3 ml blood in sodium heparin vaccutainer (green top tube) transported at room temperature
In addition to G-banding, specific staining techniques such as C-banding, DA-DAPI staining, Quinacrine fluorescence are also offered on request. Sequential FISH on G banded slides is carried out to characterize complex translocations.
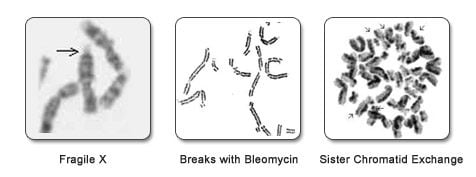
The diagnosis of chromosome breakage disorders such as Fanconi anemia, Ataxia Telangiectasia, Sister Chromatid exchange and Blooms syndrome involves addition of chromosome breakage inducing agents specific for each disorder. The test is run simultaneously with blood of a matched control. Multiple cultures of the patient and control samples are set up. A positive sample will show a higher frequency of breaks, fragile sites, radial figures or sister chromatid exchanges, compared to the control. The diagnosis of Fragile X by molecular methods has replaced cytogenetic analysis for Fragile X.
Sample: Blood (3 ml in sodium heparin) from patient and age/sex matched control transported at room temperature.
For Fanconi Anemia, 6-8ml blood should be sent in sodium heparin.
Patients with low-grade mosaicism can be detected with FISH techniques. This technique is very useful to rule out common numerical chromosome abnormalities like Down syndrome, Turner syndrome, Klinefelter Syndrome, monosomy and trisomy. Different varieties of tissues can be used such as lymphocytes from direct or cultured blood, buccal cells, urine cells, chorionic villi, placenta, cultured fibroblasts and products of conception (POC). The report is available within 2-3 days.
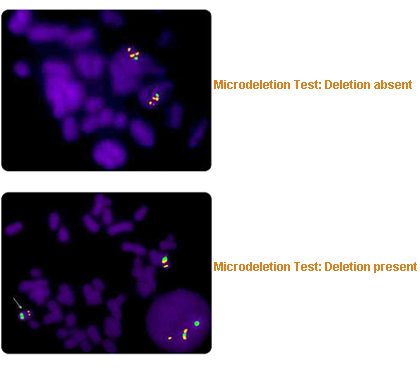
Microdeletions are often missed by karyotyping, but are easily detected by FISH on cultured lymphocytes.
Prader Willi Syndrome and Angelman Syndrome are two clinical conditions caused by a microdeletion on chromosome 15. Occasionally, these syndromes may be caused by a mutation or uniparental disomy (only one parent contributes the genetic material to the child of a particular chromosome) instead of a deletion. FISH using specific probes can pick up such cases caused by deletions.
.
Certain cases of Autism are caused by duplication of the same region on chromosome 15, instead of a deletion.
DiGeorge syndrome is caused by a microdeletion in chromosome 22 and is associated mainly with cardiac defects in children, together with cleft palate and learning problems. Seizures, hypocalcemia and hypoplasia of parathyroid glands is also known to occur (CATCH 22).
Williams syndrome is caused by a microdeletion on chromosome 7. The main clinical features are supravalvular aortic stenosis, elfin face and mental retardation.
Sample: 2-3 ml blood in sodium heparin vaccutainer (green top tube) transported at room temperature.
Beta Thalassemia is one of the commonest blood disorders in India caused by a defect in the hemoglobin (Hb) molecule which in turn leads to severe anemia. The condition necessitates frequent blood transfusion for survival. Every year 10,000 children with thalassemia major are born in India, which constitutes 10% of the total number in the world, and one out of every 8 carriers of thalassemia worldwide lives in India. There are pockets of high incidence and areas of lower incidence in our country. The specific communities with a high incidence are Kutchi Lohanas, Gujaratis, Sindhis, Punjabis, Khojas and Marwaris. Thalassemia is an autosomal recessive condition where if the abnormal Hb molecules from both the carrier parents are transmitted to the baby, then the baby is affected. If only 1 abnormal Hb molecule is present then the baby is not affected. If both the parents are carrier of 1 abnormal Hb molecule, then there are 25% chances of having an affected baby, 50% chance of having a carrier baby and 25% chance of having a totally normal baby.
Hence mutation identification is very important in cases of carrier couples before going for pregnancy. Once the mutations are identified. the couple can avail the PGT-M technology to get pregnant with an embryo which is free of thalassemia major condition. Alternatively after conceiving naturally, the fetus can be tested prenatally for the affected condition.
Periodic fever syndromes are a set of disorders characterized by recurrent episodes of systemic and organ-specific inflammation.
Periodic fever syndromes refer to diseases that cause periodic (episodic) fever that do not have an infectious (virus, bacteria) cause. In general, children with these syndromes are well between episodes. Many of these syndromes are hereditary (passed down from parents) and result from a mutation (defect or mistake) in a gene (this is the code that determines the structure of our proteins). The syndromes are defined by several factors, including:
- The gene defect
- The clinical features of the syndrome
- The parts of the body affected in addition to the fever
- The age of the child when the syndrome starts
- The ethnicity (the area of the world where the child or parents come from) of the child and parents
Many of these syndromes have a specific treatment, often based on understanding the problem caused by the genetic defect.